Chronic Inflammation Identified as Key Driver Behind Depression, Study Reveals
A groundbreaking study has revealed that chronic inflammation, not just neurotransmitter imbalances, is a significant factor in depression. This discovery reshapes traditional views of the condition, offering a more comprehensive explanation for why some patients fail to respond to standard antidepressants. The research, led by Professor Raz Yirmiya from the Hebrew University of Jerusalem, highlights the need for personalized treatments targeting inflammation, providing hope for millions worldwide.

Understanding the Study: A Comprehensive Review
The research was led by Professor Raz Yirmiya, a globally recognized expert in the field of inflammation and depression. His work has significantly advanced our understanding of how immune system dysfunction contributes to mental health disorders. The findings were published in the respected journal Brain, Behavior, and Immunity, cementing their scientific importance.
How Was the Study Conducted?
According to Neuroscience News, the study employed a systematic review of the 100 most-cited scientific papers in the field of depression and inflammation. By synthesizing decades of research, Professor Yirmiya created a detailed framework for understanding the interaction between inflammation and depression. Key methods included:
- Experimental Models: Healthy participants were injected with low doses of immune-stimulating agents to observe the onset of depressive symptoms.
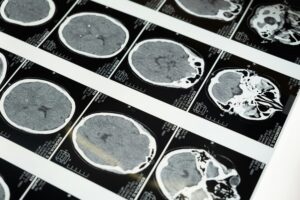
- Animal Studies: Stress models were used to study microglial activity in the brain.
- Clinical Observations: Analysis of treatment-resistant patients and vulnerable groups, such as those with chronic illnesses or early-life trauma, provided real-world insights.
The connection between depression and inflammation is not entirely new. Studies as far back as the 1980s indicated that depressed individuals often exhibit weakened immune functions. In some cases, cancer and hepatitis treatments, which provoke an inflammatory response, were shown to induce severe depressive symptoms. However, earlier research lacked the depth and mechanistic clarity that Yirmiya’s study provides.
Key Findings: A Paradigm Shift in Depression Research
The study produced several key insights that challenge traditional theories of depression:
- Inflammation as a Core Mechanism: Chronic inflammation in the body and brain plays a central role in the onset and progression of depression.
- Stress and Microglial Damage: Prolonged stress initially activates microglia but eventually leads to their degeneration, worsening depressive symptoms.
- Role of Immune-Boosting Treatments: Certain immune-stimulating treatments for cancer and hepatitis often trigger depressive symptoms, underscoring the immune system’s role in mental health.
- High-Risk Groups Identified: Vulnerable populations—including the elderly, individuals with physical illnesses, those with early-life adversity, and patients with treatment-resistant depression—are particularly prone to inflammation-linked depression.
- Potential of Anti-Inflammatory Therapies: Patients who don’t respond to standard antidepressants could benefit from treatments targeting inflammation or restoring microglial function.
Inflammation & Cognitive skills
One of the striking implications of this research is its relevance to cognitive abilities. Chronic inflammation, as identified in the study, not only drives depressive symptoms but also adversely affects cognitive functions such as memory, attention, and decision-making. The brain’s microglial cells, which play a key role in maintaining healthy neural networks, are particularly vulnerable to prolonged inflammation. When these cells are damaged by stress-induced immune responses, the resulting neuroinflammation disrupts the brain’s ability to process information effectively.
This connection explains why many individuals with depression often report symptoms like “brain fog,” difficulty concentrating, or impaired problem-solving skills. It also sheds light on why traditional antidepressants, which primarily target mood symptoms through neurotransmitter regulation, may fail to address cognitive deficits. By targeting inflammation, the study suggests that future treatments could simultaneously improve both mood and cognitive performance, offering a more holistic approach to managing depression.
Understanding this link emphasizes the broader impact of inflammation on mental health and cognitive well-being, making it a critical area for further research and therapeutic innovation.
Implications for Science, Medicine, and Society
Scientific Impact
The study fundamentally shifts our understanding of depression, emphasizing the immune system’s central role. It challenges the long-held neurotransmitter-deficiency model, which fails to explain why many patients remain unresponsive to traditional treatments.
Medical Advancements
The findings pave the way for anti-inflammatory treatments as a new frontier in depression therapy. These treatments could include:
- Immunomodulators: Medications that regulate inflammatory responses.
- Microglial Restoration: Therapies aimed at rejuvenating damaged microglia cells.
- Tailored Interventions: Personalized medicine approaches that match treatment to a patient’s specific inflammatory profile.
Societal Relevance
Depression is the leading cause of disability worldwide, affecting one in six people. By targeting the root causes of depression rather than just its symptoms, this research could drastically reduce the societal and economic burden of the condition. Improved treatments could lead to better patient outcomes, lower healthcare costs, and a reduced stigma around mental health.
Educational Significance
The study highlights the importance of educating healthcare providers about the interplay between inflammation and mental health. This knowledge could lead to earlier interventions and more precise treatment strategies.
Conclusion: A Transformative Step in Depression Research
Professor Raz Yirmiya’s research represents a paradigm shift in how we understand and treat depression. By identifying chronic inflammation as a key driver of the condition, the study provides a foundation for developing innovative, personalized treatments that address the underlying causes of depression.
For patients struggling with treatment-resistant depression, these findings offer hope. They signal a move toward therapies that not only alleviate symptoms but also tackle the root causes of mental health conditions. As this new understanding gains traction, it promises to transform despair into hope for millions affected by depression, paving the way for a brighter, healthier future.