SIDS and Sudden Infant Death Syndrome | Co-Sleeping With Your Newborn – A Complete Guide
SIDS and Sudden Infant Death Syndrome | Co-Sleeping With Your Newborn – A Complete Guide
After 9 long months of anticipation and mixed emotions, you finally get to welcome your little bundle of joy into the world. You’ve gained valuable knowledge about the pros and cons of co-sleeping vs. crib- sleeping through the hundreds of books, articles, and magazines that you’ve read. 273.75 days were spent preparing for motherhood but, you’re torn. Which do you choose? In this complete guide you will become familiar with what co-sleeping actually means, the relationship between co-sleeping and breastfeeding as well as the relationship between co-sleeping and sudden infant death syndrome, the pros and cons of co-sleeping, guidance for safe sleep and bed sharing, the relationship between co-sleeping in early childhood and social experiences during infancy, recommendations presented by the American Academy of Pediatrics (APA), the famous Parent- Infant Co-Sleeping Debate, and tips on how to stop sleeping with your newborn.
What is Co-Sleeping?
Here in the United States, a growing trend exists among families with newborn babies. Since 1993, more moms are choosing to hold their infants close throughout the night. This child-rearing practice of bedsharing, defined as infants and young children sharing a bed with their parents for sleep, has grown from about 6 percent to 24 percent in 2015.
A recent survey of over 8,000 caregivers in the United States revealed that rates of regular parent-infant co-sleeping more than doubled between 1993 and 2000, from 5.5% to 12.8%. In contrast to the rapid practice of parent-infant co-sleeping in Western societies, clinicians continue to push for separate sleeping arrangements between parents and their infants. Truth be told, it is likely that numerous parents today feel so unsupported in their decision that they feel the need to conceal their choice from their childcare doctors.

Co-Sleeping With Siblings: Is It Safe?
In a study of urban Chicago families, researchers found that parental co-sleeping is not significantly associated with infant death, but co-sleeping with someone other than a parent, such as a sibling, was associated with increased risk.
Allowing other children to co-sleep in the bed with you and your baby is totally acceptable with caution and boundaries. Do not allow toddlers or older children to sleep directly next to the infant. If other children are sharing the bed, keep your partner between them and the baby.
Co-Sleeping With a Newborn- Instinct or Tradition?
From the moment the nurse places the newborn baby on the mother’s chest, there is an instant mother-infant interaction. This early skin- to- skin contact creates a physiological need to be together immediately after birth and during the hours and days that follow. Just like the nature vs. nurture debate, co-sleeping is both an instinct and a tradition around the world.
Co-Sleeping: Instinct
According to James Mckenna, an anthropologist who has been studying infant sleep for 40 years, mothers and infants mutually gravitate towards each other for survival. Human babies are contact seekers. What they need most is their mother’s and father’s bodies. Through the eyes of Mel Konner, an anthropologist at Emory University, the practice of bed-sharing has existed way before the discovery of the human species. Konner reveals that homo sapien moms and their newborns have been sleeping together for more than 200,000 years. Modern hunter-gatherer cultures provide insight into the traditional co-sleeping behaviors of our early progenitors. Even till this day, the practice continues to be universal and widespread around the world.
Co-Sleeping: Tradition
Yale University’s Human Relation Area Files presents evidence that bed-sharing is a tradition in at least 40 percent of all documented cultures. Some cultures even think it’s cruel to separate a mom and baby at night. In one study, Mayan moms in Guatemala responded with shock and pity when they heard that some American babies sleep away from their moms. In Japan, the most common sleeping arrangement is referred to as kawa no ji or the character for the river: 川. The child is represented by the shorter line and both the mother and father are represented by the longer lines.
Western culture, then again, has a long history of separating mothers and infants at night. Historians have noted that babies from wealthy Roman families slept alongside the bed in cradles and bassinets. By the 10th century, the Catholic Church started banning” infants from the parental bed to prevent poor women from intentionally suffocating an infant whom they didn’t have resources to care for. If a mother was caught sleeping with her one-year-old infant in her bed, she was excommunication from the church.
Co-Sleeping and Breastfeeding
In the mid-1990s, Notre Dame’s James McKenna decided to figure out just what happens at night when a mom sleeps with her baby. What seemed relatively unthinkable to others was actually a relatively easy task for Mckenna and his colleagues to carry out.
To better understand the relationship between co-sleeping and breastfeeding, he transformed his laboratory into an apartment, recruited dozens of moms and babies to use in this study, and analyzed their bodies while they slept. Both the physical movements of the moms and babies were captured using infrared cameras, as well as their heart rate, breathing patterns, chest movement, body temperatures, brain waves and the carbon dioxide levels between the moms’ and babies’ faces.
What McKenna found was amazing. When the mother is breastfeeding, she positions her body around the infant that resembles a shell. Through experimental observations, he saw that the mother naturally arches her body around her baby and pulls up her knees just enough to touch the baby’s feet. Inside the “shell,” the infant hears the mother’s heartbeat and, thus, subconsciously slows down their own heart rate. Additionally, the child hears the mother’s breathing, which mirrors the sounds that the infant heard in the womb. It contains a swoosh, swoosh sound, which in turns sounds like, ‘hush, hush little baby.
“It’s no wonder nearly every culture uses a swooshing sound to soothe a crying baby.” -Mckenna
The mom’s warm breath creates little clouds of carbon dioxide around the baby’s face. In spite of the fact that this may sound unsafe for the infant, the mother’s breath fortifies the child’s breathing and reminds them to take a full breath. McKenna found that for the duration of the night, babies who were breastfed in this investigation did not move all over the bed. Instead, newborns stood laser-focused on one location basically staring at their mother’s breast almost all night. In this study, it is evident that infants have evolved to experience this closeness, night after night after night.
Studies have shown that babies who aren’t breastfed have an increased risk of Sudden Infant Death Syndrome (SIDS). Based on James Mckenna’s research, breastfeeding keeps babies and mothers in a lighter stage of sleep, which decreases the risk of SIDS and promotes a greater awareness of what the other is doing.
Co-Sleeping and Sudden Infant Death Syndrome (SIDS)
Sudden Infant Death Syndrome (SIDS) is the sudden, unexplained death of a baby younger than 1 year of age. Even after an autopsy, a thorough examination of the death scene, and an intense review of the deceased individual’s clinical history, an exact cause of this disease can remain unknown. Sometimes known as “crib death,” scientific researchers associate SIDS with deficits in the infant’s brain that control the infant’s breathing and arousal from sleep. While medical examiners have discovered a combination of sleep and environmental factors that might put your baby at risk, they’ve also identified simple measures that you can take to help protect your child from this tragic cause of death.
In a family co-sleeping with their newborn, possible causes of death are clarified by ecological components. On the off chance that the baby was born with brain deficits, low birthweight, or respiratory infections, the items in their crib and/or their sleeping position can ignite these physical issues. A blend of both sleep, environmental, and physical variables can extraordinarily build the danger of SIDS.
Albeit sudden infant death syndrome can strike any infant, scientists have recognized a few factors that may build a child’s hazard. They include:
- Sex: Boys are slightly more likely to die of SIDS.
- Age: Infants are most vulnerable between the second and fourth months of life.
- Race: For reasons that aren’t well-understood, nonwhite infants are more likely to develop SIDS.
- Family history: Babies who’ve had siblings or cousins die of SIDS are at higher risk of SIDS.
- Secondhand smoke: Babies who live with smokers have a higher risk of SIDS.
Being premature: Both being born early and having a low birth weight increase your baby’s chances of SIDS.
In the early 2000s, a few investigations found that bed-sharing considerably raised a child’s danger of SIDS. In these cases, the proof is solid and clear. Parents who drink or take drugs shouldn’t be sleeping with their infants since they could move over onto their child. Mothers who’ve just given birth to infants who are premature should not smoke or sleep in the same bed as their babies because of potential respiratory issues that can occur in the infant. Suffocation can likewise happen when babies sleep on couches since babies can be caught in between their parent and the cushions.
Peter Blair, a medical statistician at the University of Bristol, and his colleagues spent 25 years studying SIDS epidemiology. They found that a baby was 18 times more likely to die of SIDS when sleeping next to a parent who had been drinking. In another study, they found a similar risk for babies sleeping on sofas.
However, what about families who don’t drink or smoke? Whose babies aren’t premature or underweight?
In an analysis from two case-control studies in the UK, Robert Platt, a biostatistician at McGill University, examined the relationship between sudden infant death syndrome and infants who co-sleep in the absence of hazardous circumstances. One examination included 400 total SIDS cases and just 24 cases in which the infant had shared the bed without parental hazards. In the other examination, there were only 12 of these cases out of 1,472 SIDS deaths. In the last investigation, some data about the parent’s drinking propensities was missing. Nevertheless, the two examinations arrived at comparative conclusions. For babies older than 3 months of age, there was no detectable increased risk of SIDS among families that practiced bed-sharing, in the absence of other hazards. So far, only two studies have looked at this question.
Platt believes that there may be an increased risk among babies who are younger than 3 months. He further explains that if there is an increased risk, it’s probably not of a comparable magnitude to some of these other risk factors, such as smoking and drinking alcohol. In other words, the risks present in this age group do not pose as much as a risk than parents who decide to co-sleep with their children after they’ve just smoked a cigarette or drank a beer, or two. Overall, the two studies suggest bed-sharing, when no other hazards are present, raises the risk of SIDS by about threefold.
Co-sleeping and SIDS Risk Factors

- Parents who become tired easily, sleep heavily, consume alcohol or take medication that affects their level of consciousness
- Illness of either the mother or the baby: First and foremost, you must take care of your health and your baby’s health before co-sleeping with your newborn. Skin- to- skin contact easily distributes germs between the mother and her baby.
- Babies who are underweight or preterm
- Sofas and/or waterbeds
- Soft bedding and pillows
- Excessive pillows and duvet covers
- Room Temperature
- Bedding that covers the infant’s head
Smoking serves as another significant risk factor in sudden infant death syndrome. Compared to their non- smoking counterparts, babies are 15 times more likely to die from SIDS if their mothers smoke during their pregnancy. In 1998, the Department of Health conducted a survey where only 9% of women knew that smoking in pregnancy increased the risk of SIDS. The CESDI Sudden Unexpected Deaths in Infancy (SUDI) Studies found that babies who died within the first year of life were twice as likely to have been exposed to tobacco smoke, with the risk increasing with the number of hours of exposure.
The most frequent risk in bed-sharing arrangements is paternal alcohol consumption among certain social groups. Helen L. Ball found that: “the heaviest drinking bed-sharing fathers were of middle- income, socioeconomic classes III and IV, with little post-16 education, whose partners were breastfeeding their first infants.” As the numbers of babies who are breastfed increases in this section of the population, attention needs to be paid to the wider implications of these changes in infant care practices.
“The heaviest drinking bed-sharing fathers were of middle- income, socioeconomic classes III and IV, with little post-16 education, whose partners were breastfeeding their first infants.”- Helen L. Ball
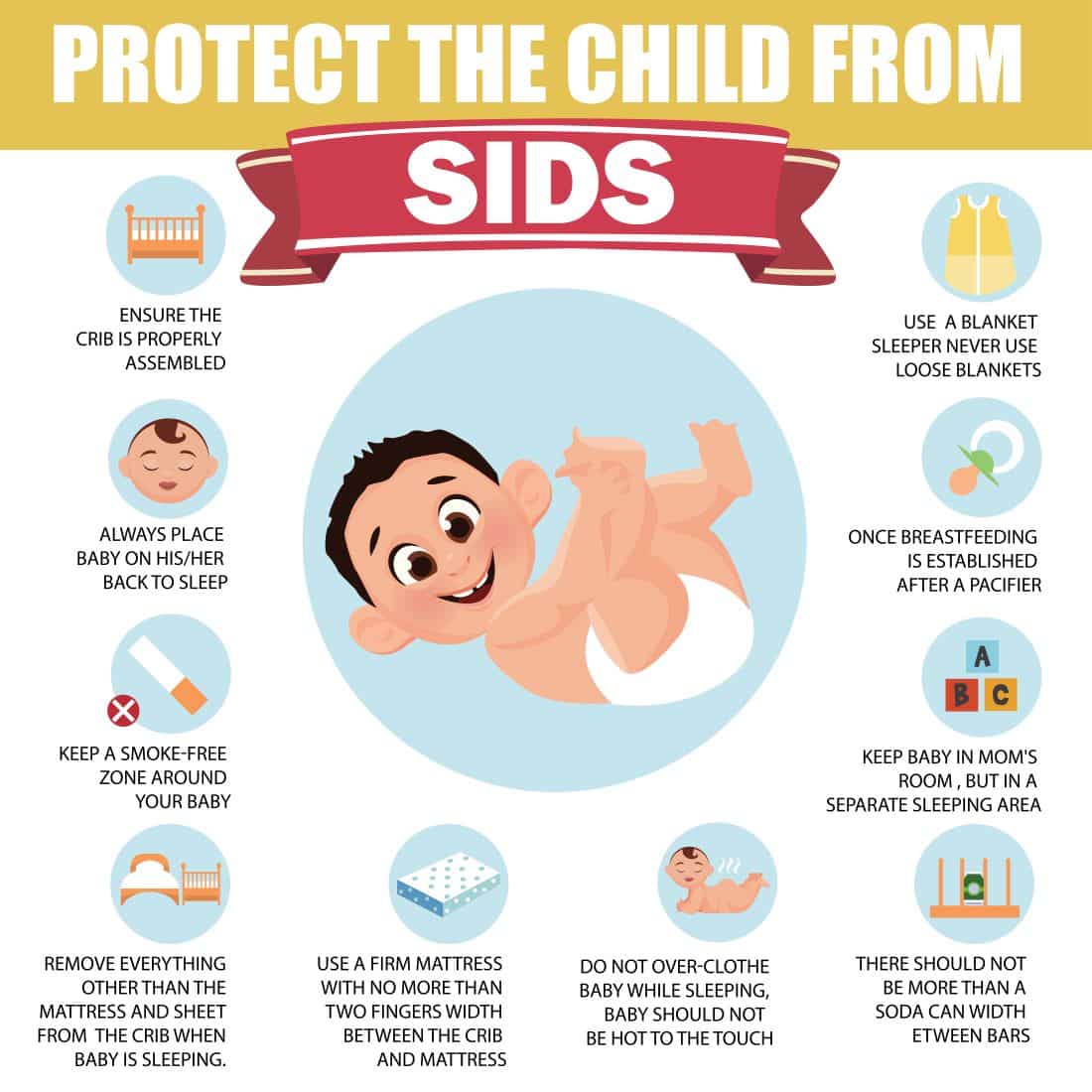
Guidance for Safe Co-Sleeping and Bed Sharing
- Keep the mattress firm: Co-sleeping should never take place on a water-bed, sofa, or old sagging mattress because this can put the infant at risk for suffocation.
- Ensure that your baby’s sleep environment is free of any gaps or small spaces
- Maintain the room temperature at a comfortable temperature – around 18°C.
- Do not overdress or swaddle your baby: Care should be taken to ensure that the baby cannot become entangled in loose ties from nightwear. Parents should keep a close eye on signs of overheating, such as sweating or the chest feeling hot to the touch, throughout the night.
- Keep pillows away from the baby
- Keep the crib bare: There is no evidence that bumper pads prevent injuries, and there is a potential risk of suffocation, strangulation or entrapment.
- If your partner is sharing the bed with you and your baby, make sure that he/she is aware that the baby is in the bed
- Never allow pets to share the bed
- Become aware of the protective “C”- shaped position for co-sleeping. This is especially important for bottle-feeding mothers
- Never co-sleep with your infant if you’re under the influence of alcohol or other drugs
- Regardless of where the infant sleeps, always place an infant on its back to sleep.
The New Zealand Strategy
Specialists have been utilizing the New Zealand Strategy for a considerable length of time and the outcomes have been tremendous. Since 2010, mortality rates have decreased as much as 30 percent in the realm of sudden infant death syndrome.
The New Zealand Strategy specifically figures out which babies are at high risk for SIDS. Through this strategy, families will not be shamed by their decision to co-sleep, rather, they’re being taught how to bed-share more safely. Doctors will talk about what increases the risk, such as drug use and alcohol use, and families are given a so-called Moses basket so that the family can bring the baby into the bed. If parents feel less judged by their doctors, then they are able to receive better advice about the dangerous circumstances surrounding SIDS.
Co-Sleeping Pros
An implied medical advantage of bedsharing is that it encourages increased frequency and duration of breastfeeding, which is broadly held to be the best strategy for nourishing youthful babies. Bedsharing promotes breastfeeding and greater bonding opportunities. While there is no current research contending that co-sleeping has a defensive impact against SIDS, James McKenna’s exploration has demonstrated that babies who sleep by their mothers exhibit positive physiological changes. These progressions can hypothetically decrease the dangers of SIDS.
Co-Sleeping Cons
Co-sleeping puts the infant at risk for sleep-related deaths, including sudden infant death syndrome, accidental suffocation, and accidental strangulation. About 3,700 babies die each year in the U.S. from sleep-related causes. From a psychiatric viewpoint, prolonged bed sharing may be considered symptomatic of maternal separation anxiety, an inability to set limits, difficulty maintaining a consistent child bedtime routine, or a disturbed mother-infant relationship.
Due to the fragmented and poor quality sleep of family members, elementary school children tend to act out and cause disruptions in family life. Concerns have been raised about the unfavorable results of bedsharing for family relations, particularly the marriage, with some warning that marital intimacy will suffer from prolonged bed sharing arrangements. Whereas bed- sharing can potentially hinder the romantic relationship between parents, there is a lack of empirical evidence to support this possible co-sleeping con. Solitary sleeping and co-sleeping families both report marital intimacy and partner satisfaction despite existing controversies.
In a study comparing both U.S. and Chinese elementary school children, the Chinese children were reported to have more sleep problems such as difficulty falling asleep, fear of sleeping in the dark, talk during sleep, and restless sleep. Although researchers clearly see that these children are suffering from the consequences of sleep disturbances, do nighttime care providers see these characteristics as problematic? Cultural considerations must be included as researchers evaluate the disruption posed by night wakings and other sleep behaviors. Parental recognitions are socially bound and essential to an evaluation of what constitutes a sleep issue. The definitions of sleep onset and night waking problems in young children are, to a certain extent, culturally determined.
Co-Sleeping and Safety Concerns
Those who are against co-sleeping argue that the practice is, in many ways, a dangerous one that, because of health, developmental, and safety concerns, has been and should continue to be abandoned by health professionals and parents. On the other side of the spectrum, some researchers contend that the practice of bedsharing is only a risk factor for SIDS if parents smoke or engage in other hazardous practices. They’ve also argued that entrapment/suffocation is only associated with bedsharing due to other contextual factors such as bed safety (soft mattresses, sleeping together on a couch) and parental variables (e.g. intoxication, smoking).
Co-Sleeping and Childhood Development
One one side of this controversial debate, some researchers argue that co-sleeping deters childhood development. They see the first year as an opportunity for infants to master sleep consolidation and sleep regulation. Other research views the process of sleep consolidation and sleep regulation as a natural process that matures over the course of the first several years of life. Controversy on whether falling asleep and staying asleep should be done naturally and independently or with the aid of parental involvement continues to reign as an issue for this field.
Co-Sleeping: Psychosocial Outcomes
Another formative issue concerns the psychosocial outcomes for children and parents of early sleep arrangements. Of prime interest is whether the requisite path towards independence and separation–individuation will be derailed for bed- sharing infants. In particular, Western societies believe that children should acquire the skills that are needed to thrive as independent individuals. This promotes the belief that ‘self-soothing’ in infants is an important developmental milestone. Co-sleeping or sleeping with a parent or sibling prevents the infant from becoming independent. Despite these convictions, evidence suggests that children who co- slept with their parents during the first year of life, are fundamentally more autonomous in everyday living abilities and in their social relations with peers as preschoolers compared to solitary sleeping children.
In their 18-year longitudinal study of conventional and nontraditional families, Okami and colleagues found that bedsharing during infancy and early childhood was unrelated to long-term problems in sleep, sexual pathology or problems in other areas of behaviour. Some sleep specialists see constant night wakings and excessive dependence on parental help for going to sleep and staying asleep in newborns and young children who co-sleep. However, in numerous nations around the globe where bedsharing is the norm, reports of rest issues are uncommon.
Co-Sleeping in Early Childhood and Social Experiences During Infancy
Marie J. Hayes, Michio Fukumizu, Marcia Troese , Bethany A. Sallinen and Allyson A. Gilles studied the relationship between co- sleeping arrangements in early childhood and social experiences during infancy. They monitored this relationship by using sleep- wake behaviors that took place during the infancy and early childhood periods from current and retrospective parental reports.
A convenience sample of 3-to 5-year-old children was obtained from the University of Maine’s Child Study Center in Orono, Maine. The Child Study Center is part of the Psychology Department at the University and provides a preschool educational experience to families who are encouraged to take interest in the preschool’s research mission. The average age of the children was 3.8 years, 51% were female, and 73% were breastfed during infancy.
Results showed that early childhood co-sleeping was reactive. Co-sleeping in early childhood was associated with sleep location in infancy (i.e. proximity to the mother’s bed) during wake–sleep transitions and night feedings. In infancy, researchers recalled an inverse relationship between the use of security objects in early childhood and current parent- seeking behaviors, night waking, poor bedtime routines, fear of the dark, and social contact during wake–sleep transitions. These findings suggest that co-sleeping in early childhood is related to social experiences during infancy, particularly the amount of parent social contact and security object use.
At 12 months old, a newborn’s proximity to the mother’s bed was related to co-sleeping at 2 and 4 years of age. Infant sleep location in a different room was related to self- soothing techniques that were practiced independently by the infant. Self-calming was additionally identified with a more prominent delay in parental intervention for night crying. Self-soothing opportunities are presented to the infant with increased proximal distance from the maternal bed, less parental awareness of infant awakenings, and longer delays in responding.
Interestingly enough, the use of a sleep aid may do more harm than good at sleep onset. In infancy, security object attachment and difficulty without the object were associated with more solitary sleeping and independent sleep onset skills in early childhood. Infants who did not use a sleep aid were associated with more co-sleeping in early childhood. In sum, you will find that infants who have more independent sleep onset skills, solid sleep routines, and low rates of nightwalking in early childhood have a history of using a sleep aid during infancy. In Western society, it’s possible that parental encouragement of object use may be simply a corollary of parental practices that are cultural conventions. These parents believe that early independent sleep onset skills are best developed by the parental delay in response to infant night crying and ritualized bedtime routines.
Tips on How to Stop Co-Sleeping With Your Baby
It is evident that co-sleeping has both its pros and cons. If you are a parent who is 100% comfortable with continuing on the co-sleeping route, that’s totally fine! But if you are a parent who wants to slowly wean you and your child off of a co-sleeping agenda, then stay tuned for these tips on how to stop co-sleeping with your baby.
Why did you begin to co-sleep with your infant in the first place? How you address this issue relies upon how and why you are co-sleeping with your infant. However, regardless of your condition, there are additional components for an effective change.
You must have a consistent nighttime routine
Is your child going to sleep in your bed every night or not? On the off chance that your child resists or you miss that feeling when your child slept close to you throughout the night, you are disturbing the establishment of a new sleeping pattern. Keep in mind that intermittent reinforcement is a powerful mechanism for encouraging undesirable behavior. According to Craig Canapari, director of the Yale Pediatric Sleep Center, the number one reason families fail at extricating their child from their bed is that they are inconsistent.
Devise a sleep time plan
Consistency requires all hands on deck. All caregivers must be aware of what this new plan consists of. If you decide that the child will not be sharing the bed with you tonight, make sure your partner is aware of this decision. Discuss with your partner where your child will sleep during the day so you are prepared to act upon this decision at night.
Agree on a “quit date”
Choose a specific date to start a change in co-sleeping behaviors.
Make solitary sleeping fun
Feelings of apprehension are completely normal for anyone who’s facing any kind of change in a normal routine. But in terms of co-sleeping, some children might feel uncertain about spending the night alone in their own bedroom without their parents. To ease this scary situation, take your child to choose a new set of pajamas or a fun bedding set. Pick out a new stuffed animal to use as a transitional object.
Face this new experience alongside your child
The beginning of a solitary sleep routine is experienced by both the child and their family. You can’t expect your child to start sleeping by themselves in an unfamiliar place right off the bat so it’s important to ease into this new situation. Craig Canapari suggests that you move with your child in their room for a week or so before starting to withdraw your presence.
Help your baby fall asleep on their own
Your child is bound to wake up at some point during the night but in order to go back to sleep without parental aid, they have to work on falling back asleep on their own. Some parents find success in checking on their baby in the middle of the night and reassuring her, without picking her up or bringing her to bed with them.
Be patient
Rest assured, co-sleeping does not last forever! Just like any other behavior, solitary sleeping becomes automatic when the correct measures are taken. Eventually, your baby will learn how to sleep on their own and your bed will become yours again.
Please do not think of yourself as a so-called “bad parent” if you choose to co-sleep with your child at any stage of their lives. This article is not meant to make you feel that you failed your children in any way because you allow them to share the bed with you at night. I hope you found the information in this article useful and helpful. Let us know what you think in the comments below!
For further reading…
In an analysis from two case-control studies in the UK, Robert Platt, a biostatistician at McGill University, examined the relationship between sudden infant death syndrome and infants who co-sleep in the absence of hazardous circumstances. One examination included 400 total SIDS cases and just 24 cases in which the infant had shared the bed without parental hazards. In the other examination, there were only 12 of these cases out of 1,472 SIDS deaths. In the last investigation, some data about the parent’s drinking propensities was missing. Nevertheless, the two examinations arrived at comparative conclusions. For babies older than 3 months of age, there was no detectable increased risk of SIDS among families that practiced bed-sharing, in the absence of other hazards. So far, only two studies have looked at this question.
Platt believes that there may be an increased risk among babies who are younger than 3 months. He further explains that if there is an increased risk, it’s probably not of a comparable magnitude to some of these other risk factors, such as smoking and drinking alcohol. In other words, the risks present in this age group do not pose as much as a risk than parents who decide to co-sleep with their children after they’ve just smoked a cigarette or drank a beer, or two. Overall, the two studies suggest bed-sharing, when no other hazards are present, raises the risk of SIDS by about threefold.
Sudden Infant Death Syndrome Risk Factors:
The risk factors for SIDS include:
- Parents who become tired easily, sleep heavily, consume alcohol or take medication that affects their level of consciousness
- Illness of either the mother or the baby: First and foremost, you must take care of your health and your baby’s health before co-sleeping with your newborn. Skin- to- skin contact easily distributes germs between the mother and her baby.
- Babies who are underweight or preterm
- Sofas and/or waterbeds
- Soft bedding and pillows
- Excessive pillows and duvet covers
- Room Temperature
- Bedding that covers the infant’s head
Sudden Infant Death Syndrome and Smoking:
Smoking serves as another significant risk factor in sudden infant death syndrome. Compared to their non- smoking counterparts, babies are 15 times more likely to die from SIDS if their mothers smoke during their pregnancy. In 1998, the Department of Health conducted a survey where only 9% of women knew that smoking in pregnancy increased the risk of SIDS. The CESDI Sudden Unexpected Deaths in Infancy (SUDI) Studies found that babies who died within the first year of life were twice as likely to have been exposed to tobacco smoke, with the risk increasing with the number of hours of exposure.
Sudden Infant Death Syndrome and Alcohol:
The most frequent risk in bed-sharing arrangements is paternal alcohol consumption among certain social groups. Helen L. Ball found that: “the heaviest drinking bed-sharing fathers were of middle- income, socioeconomic classes III and IV, with little post-16 education, whose partners were breastfeeding their first infants.” As the numbers of babies who are breastfed increases in this section of the population, attention needs to be paid to the wider implications of these changes in infant care practices.
“The heaviest drinking bed-sharing fathers were of middle- income, socioeconomic classes III and IV, with little post-16 education, whose partners were breastfeeding their first infants.”- Helen L. Ball
American Academy of Pediatrics: Recommendations on SIDS and other sleep-related infant deaths
The American Academy of Pediatrics is an association of 66,000 essential care pediatricians, pediatric therapeutic subspecialists, and pediatric surgeons. They are committed to the wellbeing, security, and prosperity of newborn children, youngsters, teenagers and youthful grown-ups.
“SIDS and Other Sleep-Related Infant Deaths: Updated 2016 Recommendations for a Safe Infant Sleeping Environment,” draws on new research and serves as the first update to Academy policy since 2011. In 2016, the American Academy of Pediatrics (AAP) expressed an opposition to bed-sharing with this statement: “It should be avoided at all times with a full-term normal-weight infant younger than 4 months.”
“It should be avoided at all times with a full-term normal-weight infant younger than 4 months.”- The American Academy of Pediatrics (APA)
Newly revised recommendations call for newborn babies to share their parents’ bedroom for the first six months and, optimally, for the first year of life. Parents should rest their baby on a firm sleep surface, such as a crib or bassinet with a tight-fitting sheet. Lori Feldman-Winter, a member on the Task Force on SIDS, says: “There should be no pillows, sheets, blankets or other items that could obstruct the infant’s breathing or cause overheating.” While infants are at an increased risk for SIDS between the ages of 1 and 4 months, new evidence demonstrates that soft bedding continues to pose hazards to babies who are 4 months and older. To guarantee a safe resting place for your baby, stay away from soft bedding, including crib bumpers, blankets, pillows and soft toys. The crib should be bare and the infant should be placed on their back. Research has shown that room-sharing decreases the risk of SIDS by as much as 50 percent.
“There should be no pillows, sheets, blankets or other items that could obstruct the infant’s breathing or cause overheating.”- Lori Feldman- Winter
Doctors strongly emphasize the importance of skin-to-skin care immediately following birth. Skin-to-skin contact ought to be limited if one, or both, parents smoke tobacco, abuse alcohol, or other illicit drugs. For this can jeopardize the infant’s health and ultimately, their life.
Breastfeeding is likewise prescribed as protection against SIDS. After feeding, the AAP urges guardians to move the infant to his or her separate sleeping space, preferably a crib or bassinet in the parents’ bedroom. Winter explains: “If you are feeding your baby and think that there’s even the slightest possibility that you may fall asleep, feed your baby on your bed, rather than a sofa or cushioned chair. If you do fall asleep, as soon as you wake up be sure to move the baby to his or her own bed.”
“If you are feeding your baby and think that there’s even the slightest possibility that you may fall asleep, feed your baby on your bed, rather than a sofa or cushioned chair. If you do fall asleep, as soon as you wake up be sure to move the baby to his or her own bed.”- Lori Feldman- Winter
Other recommendations include:
- Offer a pacifier at nap time and bedtime.
- Do not use home monitors or commercial devices, including wedges or positioners, marketed to reduce the risk of SIDS.
- Infants should receive all recommended vaccinations.
- Supervised, awake tummy time is recommended daily to facilitate development.
References
American-Academy-of-Pediatrics-Announces-New-Safe-Sleep-Recommendations-to-Protect-Against-SIDS. (n.d.).
Canapari, C. (2015, November 10). How To Stop Co-sleeping. Retrieved July 24, 2018, from https://drcraigcanapari.com/want-to-stop-cosleeping-heres-how/
Goldberg, W. A., & Keller, M. A. (2007). Parent-infant co-sleeping: why the interest and concern?.Infant & Child Development, 16(4), 331-339.
Hayes, M. J., Fukumizu, M., Troese, M., Sallinen, B. A., & Gilles, A. A. (2007). Social experiences in infancy and early childhood co-sleeping. Infant & Child Development, 16(4), 403-416. ( Study)
Is Sleeping With Your Baby As Dangerous As Doctors Say?. (2018). Morning Edition